
Raya Muttarak writes about what we have learnt about the COVID-19 outbreak so far, and how collective mitigation measures could influence the spread of the disease.
Since the outbreak of COVID-19 in Wuhan, China back in January, we have learnt a lot about the virus: we know how to detect the symptoms, and a vaccination is currently being developed. However, there are still many uncertainties:
We for example don’t know enough about the disease’s fatality rate – mainly because we don’t precisely know how many people are infected, which is the denominator. We also don’t know exactly how the virus spreads. Generally, it is assumed that the virus spreads from person-to-person through close contact (within about 1 meter) and through respiratory droplets produced when an infected person coughs or sneezes. It is also thought that COVID-19 can spread from contact with contaminated surfaces or objects.
In addition, knowledge about the timing of infectiousness is still uncertain. There is evidence that the transmission can happen before the onset of symptoms, although it is commonly thought that people are most contagious when they are most symptomatic. This information is crucial, because if we know the timing patterns of the transmission, we could adopt better measures around when to quarantine an infected person.
Lastly, we don’t yet know whether the spread of the disease will slow down once the weather gets warmer.
What is currently happening in Iran, Italy, Japan, and South Korea may be unique to these countries, but it is more than likely that most countries will eventually experience the spread of COVID-19. In this regard, epidemiologists have estimated that in the absence of mitigation measures, in the worst-case scenario, approximately 60% of the population would become infected. In February, Nancy Messonnier, the director of the Centers for Disease Control and Prevention’s National Centre for Immunization and Respiratory Diseases in the US, warned that “It’s not so much of a question of if this will happen anymore, but rather more of a question of exactly when this will happen.”
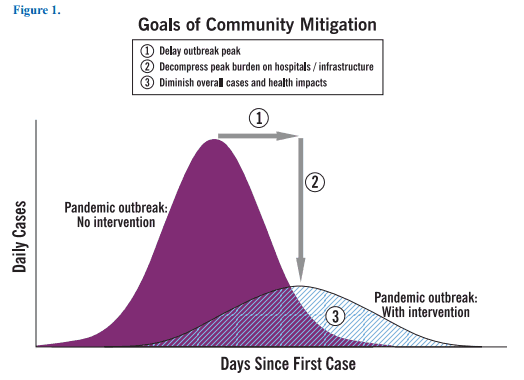
We learnt from an epidemiological transmission model that public efforts to curb the transmission of the disease should be directed towards flattening the epidemic curve. This is crucial, since the treatment of severe lung failure caused by COVID-19 requires ventilators to help patients breathe in intensive care units (ICUs). Not a single country in the world has the capacity to absorb the large number of people who would need intensive care at the same time. Experience from Italy shows that about 10% of all patients who test positive for COVID-19 require intensive care. Although efforts have been made to increase ICU capacity, the rapidly growing number of infected patients is overloading the healthcare system. Measures to reduce transmission in order to slow down the epidemic over the course of the year will therefore significantly mitigate the impact of COVID-19.
 © IIASA
© IIASA
The figure above shows the distribution of infectious cases with and without intervention. If the outbreak peak can be delayed, this allows the health system and healthcare professionals to bring the number of persons that require hospitalization and intensive care in line with the nation’s capacity to provide medical care. To flatten the epidemic curve and lower peak morbidity and mortality, calls for both government response and individual actions.
We will have to follow the protocol of the Austrian Health Ministry, but certain practices such as social distancing, washing hands, and avoiding gathering in crowded places, can help reduce the transmission of the disease. While it is true that young and healthy people are less likely to get sick and die from COVID-19, they can still be a virus carrier and thus transmit the disease to other vulnerable subgroups of the population, such as older people and those with underlying health conditions. An article recently published in The Lancet provides helpful information to better understand the current situation and explains why fighting against COVID-19 will take collective action.
Reference:
Anderson R, Heesterbeek H, Klinkenberg D, & Hollingsworth T (2020). How will country-based mitigation measures influence the course of the COVID-19 epidemic? The Lancet 0(0) DOI: 10.1016/S0140-6736(20)30567-5
Note: This article gives the views of the author, and not the position of the Nexus blog, nor of the International Institute for Applied Systems Analysis.